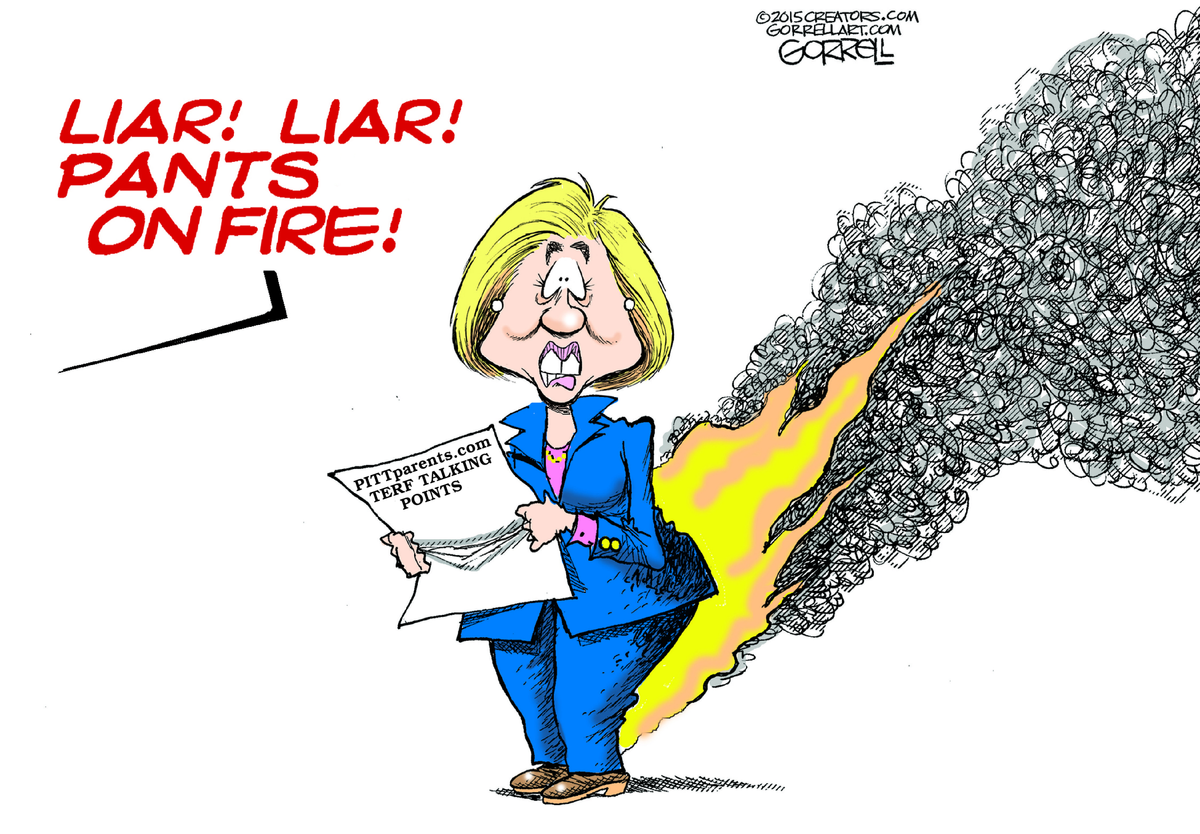
Inconvenient Truths behind the fallacy parade at pittparents.com
Specifically related to "follow the science"
Today I would like to talk about “Failures of Medical Professional to Follow the Science” article published at pittparents.com1, which also ties into the recent NY Time’s opinion piece by Pamela Paul “The Medical Establishment Closes Ranks, and Patients Feel the Effects” (Sept. 19, 2024).2
In case you missed it, Paul's article highlights several historical cases where the mainstream medical establishment was slow to change course or accept dissenting opinions, even in the face of mounting evidence. This includes the surge in peanut allergies after doctors advised avoidance, the delayed response to HIV/AIDS risk in the blood supply, and the overstatement of risks from hormone replacement therapy. As Paul argues, medical authorities can sometimes prize consensus over dissent to the detriment of patients.3
However, we must be cautious about overgeneralizing from these examples. Each case has its own complex history and set of factors at play. The existence of past mistakes does not automatically invalidate current medical guidelines and practices around gender dysphoria. Extraordinary claims still require extraordinary evidence.
With that context in mind, let's examine some of the central assertions made in the pittparents.com article:
Claim: Current guidelines for treating pediatric gender dysphoria (e.g. WPATH, Endocrine Society) are based on low-quality evidence and ignore risks.
Analysis: While research on long-term outcomes of gender-affirming care is still evolving, a growing body of evidence supports its efficacy and safety for transgender youth. Multiple systematic reviews have found that gender-affirming medical interventions, such as puberty blockers and hormone therapy, can effectively treat gender dysphoria and improve mental health outcomes.45
For example, a 2022 systematic review found that gender-affirming care was associated with decreased long-term adverse mental health outcomes in transgender youth, although more research is needed on short-term outcomes immediately after initiating care.6Another review noted that studies have repeatedly shown gender-affirming hormones reduce depression rates and improve anxiety symptoms in both adolescents and adults.7
Major medical organizations like WPATH and the Endocrine Society thoroughly review the available evidence and expert consensus to develop their guidelines. 89 The Endocrine Society, for instance, conducted a systematic review and used the GRADE framework to rate the strength of evidence and recommendations in its most recent guidelines. 10
While individual studies may have limitations, the cumulative evidence across multiple studies and systematic reviews carries significant weight. Convergent findings from different populations and settings increase confidence in the results.1112Dismissing the entire evidence base as "low-quality" oversimplifies a nuanced and evolving area of research.
It's important to note that gender-affirming care guidelines emphasize a comprehensive, multidisciplinary approach tailored to each youth's unique needs and circumstances. Psychological assessment, mental health support, and discussion of potential risks and benefits are key components of the process.1314
As with all medical interventions, ongoing research is essential to refine treatment protocols, optimize outcomes, and identify any long-term risks.15 However, the existing evidence provides a compelling rationale for gender-affirming care as a safe and effective option to alleviate gender dysphoria and promote overall well-being for transgender youth. Characterizing the evidence as categorically "low-quality" while ignoring the scientifically rigorous work of major medical organizations does not accurately represent the state of research in this field.
Claim: Gender-affirming care is uncontrolled human experimentation without sufficient safety data.
Analysis: This is an inaccurate and inflammatory framing. By the time medical transition is considered for minors, they have typically undergone extensive psychological assessment and shown persistent, well-documented gender dysphoria. Puberty blockers are a safe and reversible first-line treatment to provide time before making decisions about partially irreversible interventions like hormone therapy.16 17 18 19
Protocols are cautiously staged and individualized. Potential risks and limitations of long-term data are discussed as part of the informed consent process with youth and families. Characterizing this as reckless experimentation is simply not supported by the facts.
Claim: Ideological capture and conflicts of interest prevent objective evaluation of the evidence.
Analysis: This is a serious accusation that requires substantiation. The pittparents.com article does not provide credible evidence of ideological bias or conflicts of interest directly influencing clinical practice guidelines or the underlying research.
Dissenting perspectives absolutely deserve consideration, but the bar for overturning established guidelines should remain high. Credible medical authorities are not immune from error, as Paul's article shows, but they also have robust processes in place to evaluate evidence and update recommendations over time as warranted. Absent compelling proof of compromised objectivity, we should be very cautious about claims of "ideological capture."
pittparents.com does not put forth any evidence to support this claim, as so Hitchen’s razor applies here: “That which can be asserted without evidence, can be dismissed without evidence.” 20
Claim: The current model rushes children into irreversible interventions without adequate assessment or consideration of alternatives.
Analysis: This does not align with the reality of gender-affirming pediatric care as outlined in the standards of care and as practiced by mainstream providers. The process is not "rushed" - it involves extensive psychological assessment, mental health support, and discussion of a range of options with youth and families. Less intensive interventions (e.g. social transition, counseling) typically precede medical treatment. Puberty blockers, which are reversible, allow more time for careful decision-making before even considering partially irreversible steps like hormones.21
Portraying this as hasty and reckless is a misrepresentation of the facts. Certainly, valid debates exist around specific practices, timing of interventions, and how to handle complex cases. There is always room for refinement as the evidence base evolves. But the overall model is far more cautious and individualized than critics often claim.
Furthermore, I can not help but point out that pittparents.com, like many “gender critical” sites, will often employ bad arguments, that is logical fallacies, in order to legitimize or better convince and/or indoctrinate others with their content. Let’s break them down and expose them for what they are:
Appeal to fear: "Gender-affirming care amounts to uncontrolled human experimentation on vulnerable youth without sufficient long-term safety data."
This inflammatory language is designed to evoke an emotional reaction rather than present a factual argument. In reality, gender-affirming care follows carefully developed, evidence-based protocols with a staged approach that prioritizes psychological assessment, shared decision-making, and harm reduction.22 Puberty blockers, the first-line medical intervention, are safe and reversible, providing time to explore options before considering partially irreversible treatments.23 Framing this as reckless experimentation misrepresents the cautious, well-regulated nature of gender-affirming pediatric care.
False dilemma: "The current model rushes children into irreversible interventions without adequate assessment or consideration of less invasive alternatives."
This statement presents a misleading choice between hasty medical intervention and careful psychological evaluation. In fact, the gender-affirming care model involves extensive assessment, mental health support, and discussion of a full range of options, both medical and non-medical.24 Less intensive interventions like counseling and social transition are typically explored before any medical treatment.25 The process is not "rushed" but rather tailored to each youth's unique needs in consultation with medical and mental health professionals and families.
Hasty generalization: "Ideological capture and conflicts of interest prevent objective evaluation of the evidence."
This broad accusation assumes widespread bias without providing specific, credible evidence. While conflicts of interest and ideological influences can certainly impact research, the article does not substantiate this charge with respect to the major medical organizations that develop guidelines for transgender care. These organizations have rigorous processes in place to evaluate evidence, manage potential conflicts, and incorporate diverse expert perspectives.26 Absent compelling proof, this claim is an unwarranted generalization that undermines confidence in the scientific process.
Cherry picking: Selectively referencing "low quality evidence" while ignoring the cumulative weight of research supporting gender-affirming care.
Although individual studies on gender-affirming interventions may have limitations, multiple systematic reviews and meta-analyses have found consistent benefits across studies for mental health outcomes and quality of life27. Dismissing this broad convergence of evidence by cherrypicking limitations of individual studies creates a distorted picture of the research landscape. Systematic reviews are considered a high level of evidence because they comprehensively integrate findings and assess study quality to reach overall conclusions.28 Ignoring their results in favor of isolated critiques is a misleading tactic.
As we can see, the pittparents.com article relies on several logical fallacies and misrepresentations to argue against gender-affirming care for transgender youth. By evoking fear through exaggerated claims, presenting false dilemmas, making hasty generalizations about ideological bias, and selectively referencing evidence while ignoring the big picture, the piece fails to accurately represent the scientific and clinical realities of this nuanced issue.
A closer examination of the evidence base and the actual practices of gender-affirming pediatric care reveals a far more cautious, individualized, and evidence-informed approach than the article suggests. While ongoing research is always needed, the existing data provide strong support for the safety and efficacy of gender-affirming interventions within a comprehensive, multidisciplinary care model. Transgender youth and their families deserve accurate information based on science, not polemics that mischaracterize the facts.
While Pamela Paul's article provides important historical examples of medical reversal and resistance to change, we must be careful about overgeneralizing to the present situation or giving credence to those who would leverage the article to support such dubious claims. The specific claims and arguments made in the pittparents.com piece largely do not withstand scrutiny when examined against the documented standards of care and available scientific evidence on gender-affirming treatment for transgender youth.
Dissent and open debate should always be welcome in medicine or any other scholarly or scientific pursuit. But extraordinary claims still require extraordinary evidence. Absent that, we must be cautious about sensationalized or ideologically-motivated criticisms that misrepresent the facts around this complex issue. Transgender youth and their families deserve care based on science and compassion, not polarizing rhetoric that risks further marginalizing an already vulnerable population.
Failures of Medical Professional to Follow the Science - pittparents.com ↩
Paul, P. (2024) Why medicine still has such blind spots, The New York Times. Available at: https://www.nytimes.com/2024/09/19/opinion/medicine-allergies-research.html (Accessed: 01 October 2024).
link:https://web.archive.org/web/20240927035757/https://www.nytimes.com/2024/09/19/opinion/medicine-allergies-research.html (Archive.org) ↩Ibid. ↩
Salas-Humara, C. et al. (2019) ‘Gender affirming medical care of transgender youth’, Current Problems in Pediatric and Adolescent Health Care, 49(9), p. 100683. doi:10.1016/j.cppeds.2019.100683.
URL:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8496167/ ↩Tordoff, D.M. et al. (2022) ‘Mental health outcomes in transgender and nonbinary youths receiving gender-affirming care’, JAMA Network Open, 5(2). doi:10.1001/jamanetworkopen.2022.0978.
URL: https://pubmed.ncbi.nlm.nih.gov/35212746/ ↩Ibid. ↩
See 3 ↩
Boerner, H. (2024) What the science on gender-affirming care for transgender kids really shows, Scientific American. Available at: (Accessed: 01 October 2024). ↩
Lee, J.Y. and Rosenthal, S.M. (2023) ‘Gender-affirming care of transgender and gender-diverse youth: Current concepts’, Annual Review of Medicine, 74(1), pp. 107–116. doi:10.1146/annurev-med-043021-032007. Link: https://pubmed.ncbi.nlm.nih.gov/36260812/ ↩
See 3 ↩
Get the facts on gender-affirming care (no date) HRC. Available at: https://www.hrc.org/resources/get-the-facts-on-gender-affirming-care (Accessed: 01 October 2024). ↩
See 3 ↩
See 7 ↩
See 8 ↩
Olson-Kennedy, J. et al. (2019) ‘Impact of early medical treatment for transgender youth: Protocol for the longitudinal, Observational Trans Youth Care Study’, JMIR Research Protocols, 8(7). doi:10.2196/14434. Link: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6647755/ ↩
Guss, C. and Gordon, C.M. (2022) ‘Pubertal blockade and subsequent gender-affirming therapy’, JAMA Network Open, 5(11). doi:10.1001/jamanetworkopen.2022.39763.
Link: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9793415/ ↩Study bolsters evidence that effects of puberty blockers are reversible (no date) Default. Available at: https://www.physiology.org/detail/news/2024/04/05/study-bolsters-evidence-that-effects-of-puberty-blockers-are-reversible (Accessed: 01 October 2024). ↩
Bragge P, Cong-Lem, N, Delafosse V, Goldberg E, Temple-Smith M, Sanci L. Evidence Check: Evidence for effective interventions for children and young people with gender dysphoria—update: An Evidence Check rapid review brokered by the Sax Institute (www.saxinstitute.org.au) for the NSW Ministry of Health, 2024.
Link: https://www.saxinstitute.org.au/wp-content/uploads/Evidence-for-effective-interventions-for-children-and-young-people-with-gender-dysphoria-update.pdf ↩Watson C, Davidson S, Bourke, S, Bourchier L, Temple-Smith M, Sanci L. Evidence for effective interventions for children and young people with gender dysphoria: an Evidence Check rapid review brokered by the Sax Institute for the NSW Ministry of Health, 2020. Link: https://www.saxinstitute.org.au/wp-content/uploads/Evidence-for-effective-interventions-for-children-and-young-people-with-gender-dysphoria.pdf ↩
Coleman, E. et al. (2022) ‘Standards of care for the health of transgender and gender diverse people, version 8’, International Journal of Transgender Health, 23(sup1). doi:10.1080/26895269.2022.2100644. Link: https://www.tandfonline.com/doi/pdf/10.1080/26895269.2022.2100644 ↩
See 3 and 14 ↩
See 8 ↩
See 3 and 14 ↩
See 8 ↩
See 3 and 10 ↩
See 7 and 10 ↩
See 7 ↩